Diabetes is one of the most common chronic health conditions affecting millions worldwide, yet it is also one of the most misunderstood. Many people think diabetes is only about sugar, but in reality, it is a metabolic disorder that affects the body’s ability to process glucose properly. The good news is that diabetes education empowers individuals to understand, manage, and control the condition in a way that improves both health and quality of life.
Diabetes education is not just for those already diagnosed; it is equally important for people at risk, caregivers, families, and even communities. When people understand the causes, symptoms, and management strategies, they can take control of their health and reduce the risk of serious complications.
This guide, “Diabetes Education: Control Starts Here,” will provide everything you need to know from what diabetes is, to how you can manage it through diet, lifestyle changes, medication, and self-care. Whether you are newly diagnosed, supporting a loved one, or simply looking to learn more, this educational resource is designed to give you the tools to take charge.
What is Diabetes?
Diabetes is a chronic condition that occurs when the body cannot properly regulate blood sugar (glucose). Glucose is the body’s main source of energy, but it needs insulin a hormone produced by the pancreas to enter cells. In diabetes, either the body does not produce enough insulin or cannot use it effectively.
Types of Diabetes
- Type 1 Diabetes – An autoimmune condition where the body attacks insulin-producing cells. It usually appears in children and young adults.
- Type 2 Diabetes – The most common type, often linked to lifestyle factors. The body becomes resistant to insulin or doesn’t produce enough.
- Gestational Diabetes – Develops during pregnancy and usually resolves after birth, but increases future risk of Type 2 diabetes.
- Pre-diabetes – Blood sugar levels are higher than normal but not yet in the diabetes range. With lifestyle changes, progression can be delayed or prevented.
Why Diabetes Education Matters?
Diabetes education is not just about understanding medical facts it’s about equipping people with the skills and confidence to live healthier, more fulfilling lives. Many people diagnosed with diabetes often feel overwhelmed, but education transforms uncertainty into empowerment. It provides the knowledge needed to make informed choices every day, from what to eat to how to manage stress. With proper guidance, patients no longer see diabetes as an uncontrollable disease but as a condition they can actively manage.
1. Prevents Complications
One of the biggest benefits of diabetes education is the prevention of long-term complications. Without proper management, diabetes can lead to serious health issues such as heart disease, kidney failure, nerve damage, blindness, and even limb amputations. Education helps individuals understand why controlling blood sugar, blood pressure, and cholesterol is so important. Patients learn to recognise warning signs early and take preventive measures. Something as simple as checking feet daily or scheduling regular eye exams can prevent complications from becoming life-threatening.
2. Encourages Self-Care
Diabetes management is a daily responsibility, and education gives patients the tools to take charge. Self-care habits such as monitoring blood sugar, planning balanced meals, and engaging in regular physical activity become easier when people understand their impact. For example, knowing how certain foods raise blood sugar motivates healthier eating decisions. Learning how exercise lowers glucose helps patients stick to a fitness routine. Self-care builds independence, reducing the constant fear of relying on medical interventions.
3. Reduces Hospital Visits
When people are uneducated about diabetes, they are more likely to face emergencies like severe hypoglycaemia or dangerously high blood sugar levels. These situations often require hospitalisation, which can be stressful and expensive. Diabetes education reduces these risks by teaching patients how to handle fluctuations before they escalate. Understanding how to adjust food intake, take medications properly, and monitor glucose levels allows patients to manage their condition at home effectively. As a result, hospital admissions decrease, and overall healthcare costs are reduced.
4. Supports Emotional Health
Living with diabetes can cause anxiety, stress, and even depression. Many people worry about long-term health risks, medication costs, or the fear of complications. Diabetes education plays a vital role in emotional well-being by addressing these concerns openly. It reassures patients that they are not alone and that with proper self-management, they can live full, active lives. Support groups and counselling often included in educational programs provide a safe space to share experiences, reduce stress, and build confidence. Emotional stability, in turn, improves overall diabetes control.
5. Empowering Confidence for Life
In short, diabetes education gives people confidence to live healthier, more independent lives. Instead of feeling powerless, patients gain the knowledge to control their condition rather than letting it control them. Education creates a foundation for lifelong wellness, helping people make smarter decisions, reduce complications, and maintain a higher quality of life. Ultimately, the value of diabetes education extends beyond numbers and test results it gives people hope, strength, and the tools to thrive every day. education gives people confidence to live a healthier, more independent life.
Causes and Risk Factors
Not everyone develops diabetes for the same reasons, but common risk factors include:
- Genetics & family history – If parents or siblings have diabetes, risk increases.
- Unhealthy diet – High sugar, processed foods, and excess calories contribute to obesity and insulin resistance.
- Sedentary lifestyle – Lack of physical activity reduces the body’s ability to regulate glucose.
- Age – Risk increases after 45.
- Ethnicity – Higher prevalence in South Asians, Hispanics, African Americans, and Native Americans.
- Pregnancy – Women with gestational diabetes face higher risk later in life.
Signs and Symptoms of Diabetes
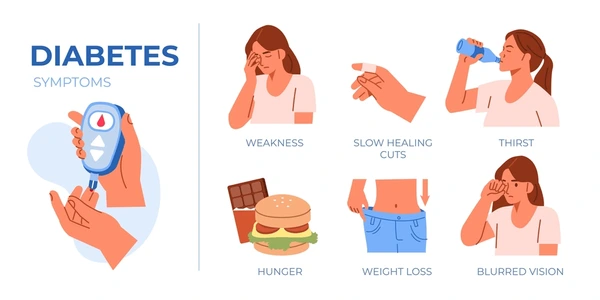
Early recognition is key. Common symptoms include:
- Excessive thirst and frequent urination
- Unexplained weight loss
- Increased hunger
- Fatigue and weakness
- Blurred vision
- Slow healing wounds
- Tingling or numbness in hands and feet
If these symptoms persist, getting tested is essential.
Diagnosis of Diabetes
Doctors use several tests to diagnose diabetes:
- Fasting Plasma Glucose (FPG) – Measures blood sugar after 8 hours of fasting.
- HbA1c Test – Reflects average blood sugar over the last 3 months.
- Oral Glucose Tolerance Test (OGTT) – Measures blood sugar response after drinking a glucose solution.
- Random Plasma Glucose Test – Checks sugar levels at any time of the day.
Diabetes Self-Management Education (DSME)
Diabetes Self-Management Education (DSME) is a patient-centred, evidence-based approach that equips individuals with the skills, confidence, and knowledge required to live well with diabetes every single day. It is not a one-time lesson but a continuous learning process that adapts to a person’s lifestyle, health status, and individual goals. The purpose of DSME is to ensure that people with diabetes don’t simply depend on doctors for every decision but instead become active participants in managing their condition. By focusing on daily behaviours and self-care, DSME empowers individuals to take charge of their health and reduce the risks of serious complications.
Core Areas of DSME
1. Nutrition and Healthy Eating
One of the most important components of DSME is nutrition. Since food directly influences blood sugar levels, patients learn how to plan meals that balance carbohydrates, proteins, and fats. Education also covers the importance of glycaemic index, portion control, and meal timing. Patients are taught practical skills like reading food labels, planning diabetes-friendly snacks, and creating meal plans that prevent sugar spikes.
2. Medications and Insulin Use
For many, managing diabetes involves oral medications, insulin, or a combination of both. DSME helps patients understand the purpose of each medication, how and when to take it, and possible side effects. Insulin training includes proper injection techniques, rotating sites, storage guidelines, and recognising when dosage adjustments may be necessary. With this knowledge, patients avoid common mistakes that could lead to hypo- or hyperglycaemia.
3. Blood Sugar Monitoring
Regular monitoring is the cornerstone of effective diabetes management. DSME teaches patients how to use glucometers and continuous glucose monitors (CGMs) accurately. It also emphasises understanding patterns—how food, exercise, stress, or illness can alter readings. By tracking glucose levels, patients can make informed decisions about diet, physical activity, and medications, preventing emergencies before they occur.
4. Physical Activity and Exercise Planning
Exercise plays a major role in lowering blood sugar and improving insulin sensitivity. DSME educates patients on safe and effective workouts tailored to their age, health condition, and fitness level. From simple daily walks to structured strength training, exercise plans are designed to fit individual lifestyles. Patients also learn how to manage blood sugar around exercise—such as checking levels before and after activity and carrying snacks in case of hypoglycaemia.
5. Stress Management
Stress and mental health are often overlooked in diabetes care, but DSME addresses them directly. Stress hormones like cortisol can raise blood sugar, making emotional health crucial. Patients are taught coping strategies such as mindfulness, relaxation techniques, breathing exercises, and building support systems. Counselling and support groups are often included in DSME programs to reduce feelings of isolation and anxiety.
6. Prevention of Complications
One of the biggest goals of DSME is long-term prevention. Education covers foot care, eye check-ups, kidney function monitoring, and heart health. Patients learn to recognise early warning signs of complications and when to seek medical help. Preventive measures reduce hospital visits, improve quality of life, and save long-term healthcare costs.
Why DSME is Life-Changing?
Diabetes can feel overwhelming, but DSME breaks it down into manageable steps. It transforms patients from passive recipients of care into confident, self-reliant managers of their health. Studies show that those who participate in DSME programs achieve better blood sugar control, experience fewer complications, and report higher satisfaction with their care.
Ultimately, DSME provides not just medical guidance but also the emotional strength to live fully with diabetes. By focusing on daily actions eating smart, monitoring blood sugar, exercising safely, managing stress, and preventing complications patients gain the power to lead healthier and more independent loveseats don’t just rely on doctors but actively take charge.
Healthy Eating for Diabetes Control
Nutrition is one of the most powerful tools in managing diabetes.
- Focus on whole grains, lean proteins, fruits, and vegetables.
- Limit refined sugars, sugary drinks, and fried foods.
- Follow the plate method: half plate vegetables, quarter lean protein, quarter whole grains.
- Learn about glycaemic index (GI) choose low-GI foods to keep blood sugar stable.
Sample Diabetes-Friendly Meal Plan
| Meal | Example Options |
|---|---|
| Breakfast | Oats with berries, boiled egg |
| Lunch | Grilled chicken, brown rice, salad |
| Snack | Nuts, Greek yoghurt, apple |
| Dinner | Baked salmon, steamed veggies, quinoa |
Physical Activity and Exercise
Exercise helps lower blood sugar and improve insulin sensitivity.
- Aerobic exercises – walking, cycling, swimming
- Strength training – builds muscle and supports metabolism
- Yoga & stretching – reduces stress and supports flexibility
Aim for 150 minutes per week of moderate activity. Always consult a doctor before starting.
Medications and Insulin Therapy
Diabetes often requires medication alongside lifestyle changes.
- Oral medications:
- Metformin (improves insulin sensitivity)
- Sulfonylureas (increase insulin release)
- SGLT2 inhibitors & GLP-1 agonists (newer options)
- Insulin therapy: Essential for Type 1, sometimes needed for Type 2. Types include rapid-acting, short-acting, and long-acting.
Education ensures patients know how to take medicines safely.
Monitoring Blood Sugar Levels

Checking sugar levels helps track progress.
- Glucometers – portable devices for self-testing
- Continuous Glucose Monitors (CGMs) – provide 24/7 real-time data
- Target Ranges: Typically 80–130 mg/dL before meals, <180 mg/dL after meals (varies individually)
Complications of Diabetes
Without proper education, diabetes can lead to serious issues:
- Short-term: Hypoglycemia (low sugar), hyperglycemia (high sugar), diabetic ketoacidosis.
- Long-term: Nerve damage (neuropathy), eye damage (retinopathy), kidney disease, heart disease, stroke.
Education reduces risks by teaching prevention.
Lifestyle Changes for Diabetes Control
- Stress management – meditation, deep breathing, hobbies.
- Sleep – at least 7–8 hours to regulate hormones.
- Avoid smoking – it worsens circulation and complications.
- Limit alcohol – excessive drinking spikes sugar.
Role of Technology in Diabetes Education
Modern technology makes diabetes education easier:
- Mobile apps for tracking meals and sugar levels
- Online communities for support
- Telemedicine consultations for remote patients
Diabetes in Children & Teenagers
Type 1 diabetes often starts in childhood. Education is vital for both parents and kids.
- Schools should support children with diabetes care plans.
- Teens face emotional challenges; counselling helps.
- Education reduces stigma and encourages healthy habits.
Pregnancy and Diabetes
Gestational diabetes needs close monitoring.
- Balanced diet and regular activity help control sugar.
- Blood sugar monitoring is essential.
- After birth, women should continue regular check-ups to prevent Type 2 diabetes.
Community and Social Support
Managing diabetes is easier with a support system.
- Diabetes educators provide training.
- Support groups reduce emotional burden.
- Families play a role by adopting healthy habits together.
Prevention of Diabetes
For Type 2 diabetes, prevention is possible.
- Maintain healthy weight
- Eat balanced meals
- Exercise regularly
- Avoid smoking and excess alcohol
- Get regular check-ups if at risk
Essential Tips for Daily Diabetes Control
Living with diabetes requires daily commitment, but with the right strategies, it becomes manageable and less overwhelming. Effective control is not about perfection it’s about consistency, awareness, and making small but impactful choices each day. Here are the essential tips for daily diabetes control that can help prevent complications, improve energy levels, and enhance overall well-being.
1. Monitor Blood Sugar Regularly
Monitoring blood glucose is the foundation of diabetes management. Regular checks help you understand how meals, exercise, stress, or medications affect your body. Using a glucometer or continuous glucose monitor (CGM) provides real-time data, allowing you to take quick action if levels go too high or low. Keeping a log of readings also helps your doctor adjust treatment plans more effectively.
2. Plan Balanced Meals
Food is directly linked to blood sugar fluctuations, making meal planning essential. A balanced meal should include complex carbohydrates, lean protein, healthy fats, and plenty of fibre. The plate method works well half your plate with non-starchy vegetables, a quarter with whole grains, and a quarter with protein. Limiting sugary drinks and refined carbs keeps blood sugar stable throughout the day.
3. Exercise Consistently
Physical activity improves insulin sensitivity and helps the body use glucose more efficiently. Aim for at least 30 minutes of moderate activity, such as brisk walking, cycling, or swimming, five days a week. Resistance training twice a week is also beneficial for building muscle and boosting metabolism. Always check blood sugar before and after exercise to avoid sudden drops.
4. Take Medications as Prescribed
Skipping medication or insulin doses can lead to dangerous fluctuations. It’s important to follow your healthcare provider’s instructions carefully. Set reminders, use pill boxes, or create a daily routine to avoid missed doses. Understanding what each medication does also gives you more confidence in managing your condition.
5. Manage Stress Effectively
Stress triggers the release of hormones like cortisol and adrenaline, which can raise blood sugar levels. Incorporating relaxation techniques such as deep breathing, yoga, meditation, or simply engaging in hobbies helps keep stress under control. Connecting with friends, support groups, or counsellors can also reduce emotional strain.
6. Prioritise Sleep
Poor sleep affects insulin sensitivity and can lead to higher blood sugar levels. Adults with diabetes should aim for 7–8 hours of quality sleep every night. Good sleep hygiene includes sticking to a regular bedtime, limiting screen time before bed, and creating a relaxing environment. Quality rest also reduces stress, supporting overall diabetes control.
7. Stay Hydrated
Water helps regulate blood sugar by aiding kidney function and flushing out excess glucose through urine. Aim for at least 8–10 glasses daily, adjusting based on activity level and climate. Avoid sugary drinks, energy beverages, and excessive caffeine, which can cause spikes and crashes in blood sugar.
8. Never Skip Check-Ups
Routine medical check-ups are critical for long-term health. Regular visits to your doctor, eye specialist, and foot care professional ensure early detection of complications. Blood tests like HbA1c, kidney function, and cholesterol checks help track overall progress. Preventive care saves both health and medical costs in the long run.
Must Read:
- What Causes Diabetes: Origins, Risks & Prevention Guide
- Diabetes Management Guidelines: Your Complete Guide to Living Better
- Nephrogenic Diabetes Insipidus: Causes, Symptoms, and Treatment
FAQs:
1. Can diabetes be cured?
Currently, diabetes cannot be completely cured. Type 1 requires lifelong insulin. Type 2 can be managed or even put into remission with lifestyle changes, but not permanently cured.
2. What foods should diabetics avoid?
Sugary drinks, processed foods, white bread, fried foods, and excessive alcohol should be avoided. Instead, focus on whole foods and balanced nutrition.
3. How often should blood sugar be checked?
Depends on the treatment plan. Those on insulin may need multiple checks daily, while others may check once or twice a week under medical guidance.
4. Is diabetes hereditary?
Yes, family history increases the risk, but lifestyle plays a huge role in Type 2 development.
5. Can exercise replace medication?
Not always. While exercise improves control, many still require medication or insulin. Always follow a doctor’s advice.
6. What is the best diet for diabetes?
A balanced diet with whole grains, lean proteins, vegetables, and limited refined sugar is ideal.
Conclusion:
Diabetes education is the foundation of effective management. By learning about the condition, patients gain the power to make healthy choices, prevent complications, and improve their quality of life. Control truly begins with awareness knowing what to eat, when to exercise, how to monitor, and when to seek help.
Families, schools, and communities all play a role in spreading awareness. With the right support, anyone living with diabetes can thrive. Remember: every step you take towards learning is a step towards better control.






